- Luca Faconti,
- Jacob George,
- Sarah Partridge,
- Carmen Maniero,
- Abilash Sathyanarayanan,
- Spoorthy Kulkarni,
- Vikas Kapil,
- Alfredo Petrosino,
- Philip Lewis,
- Terry McCormack,
- Neil R. Poulter,
- Anthony Heagerty &
- Ian B. Wilkinson
Journal of Human Hypertension volume 39, pages1–14 (2025)Cite this article
- 1200 Accesses
- 1 Altmetric
- Metricsdetails
Abstract
People living with resistant hypertension (RH) are at high risk of adverse cardiovascular events. The British and Irish Hypertension Society has identified suspected RH as a condition for which specialist guidance may improve rates of blood pressure control and help clinicians identify those individuals who may benefit from specialist review. In this position statement we provide a practical approach for the investigation and management of adults with RH. We highlight gaps in the current evidence and identify important future research questions. Our aim is to support the delivery of high-quality and consistent care to people living with RH across the UK and Ireland.
Introduction
Hypertension remains the single most important modifiable risk factor for cardiovascular disease (CVD), disability and death in the world [1, 2]. An estimated 30% of adults in the UK have hypertension, and at least 1/3rd of them fail to achieve the recommended blood pressure (BP) targets despite therapeutic intervention [3]. Such individuals have a 50% greater risk of CVD and kidney disease compared to those who achieve target BP [4]. Although BP measurement errors, lifestyle factors, suboptimal treatment strategies and undiagnosed secondary hypertension may explain poor BP control in some individuals, a proportion of people present with true resistant hypertension (RH) and remain at increased risk of CVD [4,5,6,7,8].
The British and Irish Hypertension Society (BIHS) has identified suspected RH as condition for which specialist guidance may help improve rates of BP control and help clinicians identify those people who may benefit from specialist review. In this statement, we outline the BIHS recommendations for the investigation and management of adults living with RH, based on a critical review of the literature and expert opinion where evidence is lacking. Practical approaches are described to facilitate the delivery of high-quality and consistent care across the UK and Ireland.
Definition of resistant hypertension
Despite being a common clinical condition there is no universally agreed definition of RH. The National Institute of Clinical Excellence (NICE) defines RH in adults, as BP that remains uncontrolled (i.e., office BP ≥ 140/90 mmHg/out-of-office ≥135/85 mmHg) despite taking optimal tolerated doses of an angiotensin converting enzyme inhibitor (ACE-I) or angiotensin receptor blocker (ARB) in addition to a calcium channel blocker (CCB) and a thiazide-like diuretic [9]. Confirming adherence to antihypertensive agents is also advised. The European Society for Hypertension (ESH) defines RH as clinic BP measurements ≥ 140/90 mmHg, confirmed by out-of-office measurements (24-h ambulatory BP monitor (ABPM) readings ≥130/80 mmHg) despite use of a 3-drug antihypertensive regimen including a diuretic. Evidence of adherence to therapy and exclusion of secondary forms of hypertension are also needed to confirm a diagnosis of RH [10]. The ESH guidelines are endorsed by the International Society of Hypertension [11] and their definition of RH is similar to the one proposed by the European Society of Cardiology (ESC) guidelines for the management of elevated blood pressure and hypertension [12]. The American Heart Association (AHA) [13] and Hypertension Canada [14] guidelines also specify the use of three antihypertensive agents, ‘commonly including’ and ‘preferably including’ a diuretic respectively. The AHA scientific statement on RH (2018) [15] also includes a separate category of people with BP at target on four or more antihypertensive agents, referred to as ‘controlled RH’. The rationale for the inclusion of this category is to identify people at higher risk of adverse CVD outcomes, secondary hypertension, and antihypertensive agent-related adverse effects.
In this position statement the BIHS defines RH as uncontrolled clinic BP (≥140/90 mmHg) in people with confirmed elevated out-of-office values (average daytime ABPM or HBPM ≥ 135/85 mmHg) despite appropriate lifestyle measures and treatment with optimal (or maximum tolerated) dose of at least 3 antihypertensive drugs ideally including an ACE-I/ARB, a CCB and a thiazide-like diuretic, and exclusion of both non-adherence to antihypertensive treatment and secondary causes of hypertension (Table 1).
The BIHS note that people in whom BP is controlled on more than 3 antihypertensive drugs may also benefit from a review in a specialist setting. This will ensure that pseudo-resistant and secondary hypertension are excluded, and optimal drugs and doses are prescribed, thus avoiding potential over-treatment.
Prevalence, heritability and pathophysiological aspects of RH
Prevalence
The reported prevalence of RH varies considerably due to different definitions, clinical settings and populations studied. Moreover, the diagnosis of RH is often made incorrectly [16]. Among treated adults with hypertension the prevalence of RH is reported as between 5% and 30% [17,18,19]. Population-based studies often report a prevalence between 12% and 15% with a higher percentage reported when individuals at elevated CVD risk are included [20,21,22,23]. However, using the BIHS definition of RH the estimated prevalence is more likely to be nearer 5–10%.
Heritability
Conclusive evidence regarding the heritability of RH is lacking which is unsurprising given that monogenic forms of hypertension are rare and most studies exploring candidate genes for RH have multiple methodological limitations [24,25,26].
Pathophysiology
The pathophysiology of RH is complex and both inherited and environmental factors are likely to contribute to salt and water retention, which in turn contribute to volume expansion, raised peripheral resistance and increased arterial stiffness, via the interplay of neurohormonal factors including raised aldosterone, vasopressin and sympathetic activity [27]. These factors are likely to contribute to higher rates of hypertension mediated organ damage (HMOD), chronic kidney disease (CKD) and premature CVD events.
Management of people with RH
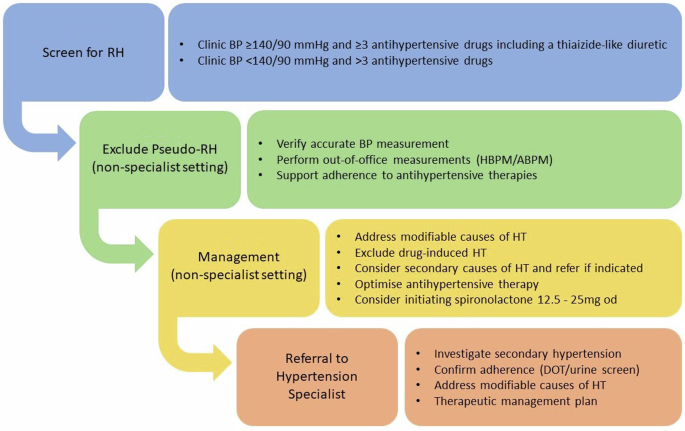
The BIHS recommend a practical approach to the investigation and management of people with RH (Fig. 1).
Screen for RH
In primary care and community-based settings, people with either suspected RH (e.g., elevated clinic BP and treatment with at least 3 antihypertensive drugs including a thiazide-like diuretic) or those at BP target on more than 3 antihypertensive drugs, can be identified by performing routine searches of electronic patient records, regular health checks, and by opportunistic encounters.
Read more on, nature.com
